


Immersive Virtual Reality (VR) technologies have continued to evolve over the past 20 years, showing their utility in a variety of clinical settings. Now, the use of VR is being increasingly seen as a way to reduce levels of pain and distress during minor medical procedures, without the use of drugs like opioids (Grassini, 2022).
The use of VR as an analgesic (pain relieving) procedure is primarily based on the fact that the perception of pain requires attentional resources. However, humans have limited attentional capacity (Kahneman, 1973). Being immersed and interacting with a virtual world offers a unique opportunity to attract a substantial amount of the patient’s limited controlled attentional resources (Hoffmann et al., 2011), leaving less attention available to process incoming pain signals.
The distractive, hypoalgesic (pain relieving) effects of VR are assumed to result from a competition for limited shared attentional resources between the immersive and interactive properties of VR and incoming nociceptive (pain-related) signals (Gupta et al., 2018). Drawing the patients’ attention away from a painful or annoying stimulus and focusing it in a relaxing virtual world, is an evidence-based intervention that has been proved to be largely effective and safe to mitigate the experience of pain and anxiety in patients undergoing painful or disturbing procedures (Chan et al., 2018; Kenney & Milling, 2016; Malloy & Milling, 2010; Mallari et al., 2019; Georgescu et al., 2020; Scheffer et al., 2018; Trost et al., 2021). In addition, some studies have already indicated a linear relationship between the sense of being inside a virtual environment (an illusion that is usually called “sense of presence”) and the effectiveness of VR distraction analgesia (Hoffman et al., 2003; Hoffman et al., 2004a).
The above-mentioned studies imply that:
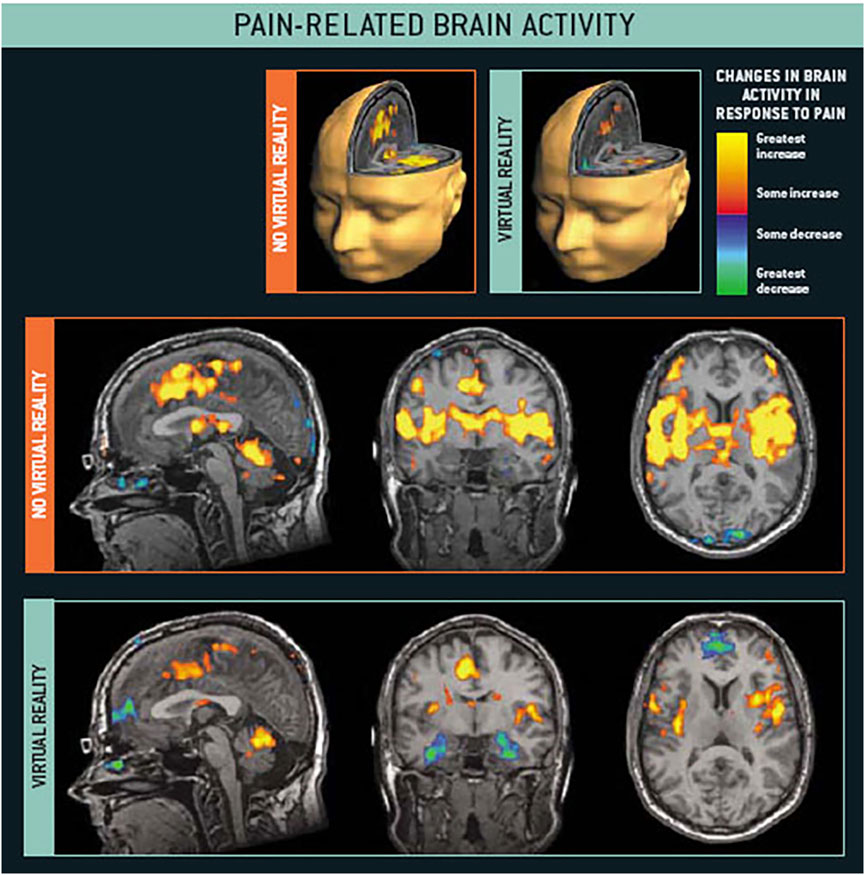
Studies have also demonstrated that exposure to VR environments reduces pain-related activity in the five regions of the brain associated with pain processing (anterior cingulate cortex, primary and secondary somatosensory cortex, insula, and thalamus) (Hoffman et al., 2004b). Thus, nowadays there is robust scientific evidence showing that VR is a safe, convenient, accessible, and effective strategy to reduce negative emotions during painful and unpleasant procedures.
VR has started to be used by patients of all ages to improve the patient experience and to provide an immersive method of distraction and relaxation during painful or uncomfortable procedures. Nowadays, different randomized controlled studies have confirmed the safety and efficacy of VR as an analgesic (pain-relieving) tool, showing its efficacy in six main clinical settings:
In general, current research studies are demonstrating that VR-based distraction interventions for procedural pain, compared to the most common procedures, can be effective in: 1) Reducing the affective and cognitive components of pain and 2) Decreasing negative emotions like anxiety and distress. However, despite those promising results, most of the existing studies are still based on small trials (Georgescu et al., 2020). In the future, larger studies need to be conducted, using more accessible VR devices, and to compare its efficacy with the most traditional methods of distraction.

One of the most common medical procedures in hospital settings is inserting a peripheral intravenous catheter or needle. This procedure is mainly used for therapeutic purposes such as the delivery of medications, drugs, fluids, and blood products (Catudal, 1999). However, it can cause high levels of distress and pain. For example, patients with conditions such as myasthenia gravis, multiple sclerosis and other neuromuscular disorders can spend up to eight hours receiving this kind of service for their condition.
Beyond clinical scenarios, intravenous procedures have also grown in relevance and popularity as an alternative way to provide micronutrients (such as vitamins, minerals, etc.) to the general population. Today, a growing number of wellness companies are promoting the transformative effects of intravenous therapy for general detoxification, vitality, and improved overall health and wellness.
In both hospital and non-clinical settings, failure to manage anxiety and pain during infusion therapy causes difficulties for healthcare providers in completing their procedures and reduces success rates (Parker et al., 2017). In addition, the experience of negative feelings increases fear, and avoidance of future intravenous and needle-related procedures (Birnie et al., 2018). However, a variety of studies have already proved the strong analgesic effect of VR during intravenous procedures, resulting in a better experience and more satisfied patients:
Relax VR combines exposure to virtual natural scenes, guided meditations, binaural beats and organic essential oils to enhance the user’s positive emotions and decrease distressing thoughts and emotions. It has a number of unique features that makes it an effective and reliable resource for reducing the levels of pain and discomfort in medical and non-clinical settings:
Recent research studies have shown the efficacy of Relax VR to reduce the levels of acute pain in clinical settings (Ju In Chan et al., 2020) and to increase pain tolerance in experimental conditions (Krainbuhl et al., 2022). Scientific studies have also proved its utility to reduce negative emotions in hospital scenarios like intensive care units (Ong et al., 2020), palliative care settings (Callistus Nwosu et al., 2021), cardiac rehabilitation units (Maciołek et al., 2020) and pre-operative contexts (Ju In Chan et al., 2020).
The above-mentioned studies suggest that Relax VR can be a good non-pharmacological analgesic for pain management during procedures that are usually associated with pain, distress or discomfort.
Basak, T., Duman, S., & Demirtas, A. (2020). Distraction-based relief of pain associated with peripheral intravenous catheterisation in adults: a randomised controlled trial. Journal of Clinical Nursing, 29(5-6), 770-777. DOI: https://doi.org/10.1111/jocn.15131
Bentsen, B., Svensson, P., & Wenzel, A. (2001). Evaluation of effect of 3D video glasses on perceived pain and unpleasantness induced by restorative dental treatment. European Journal of Pain (London, England) 5(4), 373–378. DOI: https://doi.org/10.1053/eujp.2001.0256
Birnie, K.A., Noel, M., Chambers, C.T., Uman, L.S., & Parker, J.A. (2018). Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database of Systematic Reviews, 10(10):CD005179. DOI: https://doi.org/10.1002/14651858.CD005179.pub4
Brown, P., Powell, W., Dansey, N., Al-Abbadey, M., Stevens, B., & Powell, V. (2022). Virtual Reality as a Pain Distraction Modality for Experimentally Induced Pain in a Chronic Pain Population: An Exploratory Study. Cyberpsychology, Behavior and Social Networking, 25(1), 66-71. DOI: https://doi.org/10.1089/cyber.2020.0823
Brown, N.J., Kimble, R.M., Rodger, S., Ware, R.S., & Cuttle, L. (2014). Play and heal: randomized controlled trial of DittoTM intervention efficacy on improving re-epithelialization in pediatric burns. Burns, 40(2), 204–213. DOI: https://doi.org/10.1016/j.burns.2013.11.024
Callistus Nwosu, A., Mills, M., Roughneen, S., Stanley, S., Chapman, L., & Mason, S.R. (2021). Virtual reality in specialist palliative care: a feasibility study to enable clinical practice adoption. BMJ Supportive & Palliative Care, bmjspcare-2020-002327. DOI: https://doi.org/10.1136/bmjspcare-2020-002327
Carrougher, G.J., Hoffman, H.G., Nakamura, D., Lezotte, D., Soltani, M., Leahy, L., Engrav, L.H., & Patterson, D.R. (2009) The effect of virtual reality on pain and range of motion in adults with burn injuries. Journal of burn care & research : official publication of the American Burn Association 30(5), 785–791. DOI: https://doi.org/10.1097/BCR.0b013e3181b485d3
Catudal, J.P. (1999) Pediatric IV therapy: actual practice. Journal of Vascular Access Devices, 4(1), 27-29. DOI: https://doi.org/10.2309/108300899775703652
Chan, E., Foster, S., Sambell, R., & Leong, P. (2018). Clinical efficacy of virtual reality for acute procedural pain management: A systematic review and meta-analysis. PLOS ONE, 13(7), e0200987. DOI: https://doi.org/10.1371/journal.pone.0200987
Chan, E.A., Chung, J.W., Wong, T.K., Lien, A.S. & Yang, J.Y. (2007). Application of a virtual reality prototype for pain relief of pediatric burn in Taiwan. Journal of Clinical Nursing 16, 786–793. DOI: https://doi.org/10.1111/j.1365-2702.2006.01719.x
Chen, Y-J., Cheng, S-F., Lee, P-C., Lai, C-H., Hou, I-C., & Chen, C-W. (2020). Distraction using virtual reality for children during intravenous injections in an emergency department: A randomised trial. Journal of Clinical Nursing, 29(3-4), 503-510. DOI: https://doi.org/10.1111/jocn.15088
Dabu-Bondoc, S., Vadivelu, N., Benson, J., Perret, D., & Kain, Z. N. (2010). Hemispheric synchronized sounds and perioperative analgesic requirements. Anesthesia & Analgesia, 110(1), 208–210. DOI: https://doi.org/10.1213/ANE.0b013e3181bea424
Easterlin, M.C., Berdahl, C.T., Rabizadeh, S., Spiegel, B., Agoratus, L., Hoover, C., & Dudovitz, R. (2020). Child and Parent Perspectives on the Acceptability of Virtual Reality to Mitigate Medical Trauma in an Infusion Center. Maternal and Child Health Journal, 24, 986–997. DOI: https://doi.org/10.1007/s10995-020-02955-x
Ecsy, K., Jones, A., & Brown, C. (2017). Alpha-range visual and auditory stimulation reduces the perception of pain. European Journal of Pain, 21(3), 562–572. DOI: https://doi.org/10.1002/ejp.960
Elwardy, M., Zepernick, H-J., Hu, Y., Chu, T.M.C., & Sundstedt, V. (2020). Evaluation of Simulator Sickness for 360° Videos on an HMD Subject to Participants’ Experience with Virtual Reality. 2020 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW), 477-484. DOI: https://doi.org/10.1109/VRW50115.2020.00100
Frere, C.L., Crout, R., Yorty, J., & McNeil, D.W. (2001). Effects of audiovisual distraction during dental prophylaxis. Journal of the American Dental Association, 132(7), 1031–1038. DOI: https://doi.org/10.14219/jada.archive.2001.0309
Georgescu, R., Fodor, L.A., Dobrean, A., & Cristea, I.A. (2020). Psychological interventions using virtual reality for pain associated with medical procedures: a systematic review and meta-analysis. Psychological Medicine, 50(11), 1795-1807. DOI: https://doi.org/10.1017/s0033291719001855
Gerçeker, G.Ö., Binay, Ş., Bilsin, E., Kahraman, A., & Yılmaz, H.B. (2018). Effects of virtual reality and external cold and vibration on pain in 7- to 12-year-Old children during phlebotomy: a randomized controlled trial. Journal of Perianesthesia Nursing: Official Journal of the American Society of PeriAnesthesia Nurses 33(6), 981–989. DOI: https://doi.org/10.1016/j.jopan.2017.12.010
Gerçeker, G.Ö., Bektaş, M., Aydınok, Y., Ören, H., Ellidokuz, H., & Olgun, N. (2021). The effect of virtual reality on pain, fear, and anxiety during access of a port with huber needle in pediatric hematology-oncology patients: Randomized controlled trial. European Journal of Oncology Nursing, 50:101886. DOI: https://doi.org/10.1016/j.ejon.2020.101886
Gershon, J., Zimand, E., Pickering, M., Rothbaum, B.O., & Hodges, L. (2004). A pilot and feasibility study of virtual reality as a distraction for children with cancer. Journal of the American Academy of Child and Adolescent Psychiatry 43(10), 1243–1249. DOI: https://doi.org/10.1097/01.chi.0000135621.23145.05
Gold, J.I., Soo Hoo, M., Laikin, A.M., Lane, A.S., & Klein, M.J. (2021). Effect of an Immersive Virtual Reality Intervention on Pain and Anxiety Associated With Peripheral Intravenous Catheter Placement in the Pediatric Setting: A Randomized Clinical Trial. JAMA Network Open, 4(8):e2122569. DOI: https://doi.org/10.1001/jamanetworkopen.2021.22569
Gold, J.I., Kim, S.H., Kant, A.J., Joseph, M.H., & Rizzo, A. (2006). Effectiveness of Virtual Reality for Pediatric Pain Distraction during IV Placement. Cyberpsychology & Behavior, 9(2), 207-212. DOI: https://doi.org/10.1089/cpb.2006.9.207
Goldman, R.D., & Behboudi, A. (2021). Virtual reality for intravenous placement in the emergency department—a randomized controlled trial. European Journal of Pediatrics, 180, 725–731. DOI: https://doi.org/10.1007/s00431-020-03771-9
Gold, J.I., Kim, S.H., Kant, A.J., Joseph, M.H., & Rizzo, A.S. (2006). Effectiveness of virtual reality for pediatric pain distraction during i.v. placement. Cyberpsychology & Behavior, 9(2), 207–212. DOI: https://doi.org/10.1089/cpb.2006.9.207
Gold, J.I. & Mahrer, N.E.(2018). Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. Journal of Pediatric Psychology 43(3), 266–275. DOI: https://doi.org/10.1093/jpepsy/jsx129
Grassini, S. (2022). Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. International Journal of Environmental Research and Public Health, 19, 4071. DOI: https://doi.org/10.3390/ijerph19074071
Guo, C., Deng, H., & Yang, J. (2015). Effect of virtual reality distraction on pain among patients with hand injury undergoing dressing change. Journal of Clinical Nursing 24, 115–120. DOI: https://doi.org/10.1111/jocn.12626
Gupta, A., Scott, K., & Dukewich, M. (2018). Innovative technology using virtual reality in the treatment of pain: does it reduce pain via distraction, or is there more to it? Pain Medicine, 19(1), 151-159. DOI: https://doi.org/10.1093/pm/pnx109
Hoffmann, H.G., Chambers, G.T., Meyer, W.J., Arceneaux, L.L., Russell, W.J., Seibel, E.J., Richards, T.L., Sharar, S.R., & Patterson, D.R. (2011). Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals of Behavioral Medicine, 41(2), 183-191. DOI: https://doi.org/10.1007/s12160-010-9248-7
Hoffman, H.G., Patterson, D.R., Seibel, E., Soltani, M., Jewett-Leahy, L., & Sharar, S.R. (2008). Virtual reality pain control during burn wound debridement in the hydrotank. The Clinical Journal of Pain, 24, 299–304. DOI: https://doi.org/10.1097/AJP.0b013e318164d2cc
Hoffman, H.G., Garcia-Palacios, A., Kapa, V.A., Beecher, J., & Sharar S,R. (2003). Immersive virtual reality for reducing experimental ischemic pain. International Journal of Human-Computer Interaction, 15(3), 469–486. DOI: https://doi.org/10.1207/S15327590IJHC1503_10
Hoffman, H.G., Sharar, S.R., Coda, B., Everett, J.J., Ciol, M., Richards, T., & Patterson, D.R. (2004a). Manipulating presence influences the magnitude of virtual reality analgesia. Pain, 111(1), 162-168. DOI: https://doi.org/10.1016/j.pain.2004.06.013
Hoffman, H.G.,Richards, T.L., Coda, B., Bills, A.R., Blough, D., Richards, A.L., & Sharar, S.L. (2004b). Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport, 15(8), 1245-1248. DOI: https://doi.org/10.1097/01.wnr.0000127826.73576.91
Hoffman, H.G., Patterson, D.R., Carrougher, G.J., & Sharar, S.R. (2001). Effectiveness of virtual reality-based pain control with multiple treatments. The Clinical Journal of Pain 17(3), 229–235. DOI: https://doi.org/10.1097/00002508-200109000-00007
Hoffman, H.G., Patterson, D.R., & Carrougher, G.J. (2000). Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. The Clinical Journal of Pain, 16(3), 244–250. DOI: https://doi.org/10.1097/00002508-200009000-00010
Hua, Y., Qiu, R., Yao, W-Y., Zhang, Q., & Chen X-L (2015). The Effect of Virtual Reality Distraction on Pain Relief During Dressing Changes in Children with Chronic Wounds on Lower Limbs. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses 16, 685–691. DOI: https://doi.org/10.1016/j.pmn.2015.03.001
Huang, M.Y., Scharf, S., & Chan, P.Y. (2020). Effects of immersive virtual reality therapy on intravenous patient-controlled sedation during orthopaedic surgery under regional anesthesia: A randomized controlled trial. PLoS ONE 15(2):e0229320. DOI: https://doi.org/10.1371/journal.pone.0229320
JahaniShoorab, N., Ebrahimzadeh Zagami, S., Nahvi, A., Mazluom, S.R., Golmakani, N., Talebi, M., & Pabarja, F. (2015). The effect of virtual reality on pain in primiparity women during episiotomy repair: a randomize clinical trial. Iranian Journal of Medical Sciences 40(3), 219–224. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4430883/
Jeffs, D., Dorman, D., Brown, S., Files, A., Graves, T., Kirk, E., Meredith-Neve, S., Sanders, J., White, B., & Swearingen, C.J. (2014). Effect of virtual reality on adolescent pain during burn wound care. Journal of Burn Care & Research: Official Publication of the American Burn Association 35(5), 395–408. DOI: https://doi.org/10.1097/BCR.0000000000000019
Ju In Chan, J., Teng Yeam, C., Min Kee, H., Wen Tan, C., Sultana, R., Tiong Heng Sia, A., & Leong Sng, B. (2020). The use of pre-operative virtual reality to reduce anxiety in women undergoing gynecological surgeries: a prospective cohort study. BMC Anesthesiology, 20(1):261. DOI: https://doi.org/10.1186/s12871-020-01177-6
Kahneman, D. (1973). Attention and effort. Englewood Cliffs, NJ: Prentice-Hall.
Kenney, M.P., & Milling, L.S. (2016). The effectiveness of virtual reality distraction for reducing pain: A meta-analysis. Psychology of Consciousness: Theory, Research, and Practice, 3(3), 199–210. DOI: https://doi.org/10.1037/cns0000084
Kipping, B., Rodger, S., Miller, K., & Kimble, R.M. (2012). Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns: Journal of the International Society for Burn Injuries 38(5), 650–657. DOI: https://doi.org/10.1016/j.burns.2011.11.010
Konstantatos, A.H., Angliss, M., Costello, V., Cleland, H., & Stafrace, S. (2009). Predicting the effectiveness of virtual reality relaxation on pain and anxiety when added to PCA morphine in patients having burns dressings changes. Burns: Journal of the International Society for Burn Injuries 35(4), 491–499. DOI: https://doi.org/10.1016/j.burns.2008.08.017
Krainbuhl, W. C., Maria Moroni, V. ., Legeren, A. L., Alsina Jurnet, I., & Bueno, A. M. (2022). Acute Pain Management in Virtual Environments: The Effect of a Therapeutic Narrative. Neuropsicología Latinoamericana, 14(2), 21–31. Available at: https://www.neuropsicolatina.org/index.php/Neuropsicologia_Latinoamericana/article/view/772
Kurdi, M.S. & Gasti, V. (2018). Intraoperative Meditation Music as an Adjunct to Subarachnoid Block for the Improvement of Postoperative Outcomes Following Cesarean Section: A Randomized Placebo-controlled Comparative Study. Anesthesia, Essays and Researches, 12(3), 618-624. DOI: https://doi.org/10.4103/aer.AER_114_18
Lamadah, S.M., & Nomani, I. (2016). The effect of aromatherapy massage using lavender oil on the level of pain and anxiety during labour among primigravida women. American Journal of Nursing Science, 5(2), 37-44. DOI: https://doi.org/10.11648/j.ajns.20160502.11
Lee, H.N., Bae, W., Park, J.W., Jung, J.Y., Hwang, S., Kim, D.K., & Kwak, Y.H. (2021). Virtual reality environment using a dome screen for procedural pain in young children during intravenous placement: A pilot randomized controlled trial. PLoS ONE 16(8): e0256489. DOI: https://doi.org/10.1371/journal.pone.0256489
Litwin, S.P., Nguyen, C., Hundert, A., Stuart, S., Liu, D., Maguire, B., Matava, C., & Stinson, J. (2021). Virtual Reality to Reduce Procedural Pain During IV Insertion in the Pediatric Emergency Department: A Pilot Randomized Controlled Trial. The Clinical Journal of Pain, 37(2), 94-101. DOI: https://doi.org/10.1097/AJP.0000000000000894
Maani, C.V., Hoffman, H.G., Morrow, M., Maiers, A., Gaylord, K., McGhee, L.L., & DeSocio, P.A. (2011). Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. The Journal of Trauma 71, S125–S130. DOI: https://doi.org/10.1097/TA.0b013e31822192e2
Maciołek, J., Wąsek, W:, Kamiński, B., Piotrowicz, K., & Krzesińsk, P. (2020). The impact of mobile virtual reality-enhanced relaxation training on anxiety levels in patients undergoing cardiac rehabilitation. Kardiologia Polska, 78(10):1032-1034. DOI: https://doi.org/10.33963/KP.15528
Mallari, B., Spaeth, E. K., Goh, H., & Boyd, B.S. (2019). Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. Journal of Pain Research, 12, 2053–2085. DOI: https://doi.org/10.2147/jpr.s200498
Malloy, K.M., & Milling, L.S. (2010). The effectiveness of virtual reality distraction for pain reduction: A systematic review. Clinical Psychology Review, 30(8), 1011–1018. DOI: https://doi.org/10.1016/j.cpr.2010.07.001
Miller, K., Rodger, S., Bucolo, S., Greer, R., & Kimble, R.M. (2010). Multi-modal distraction. Using technology to combat pain in young children with burn injuries. Burns: Journal of the International Society for Burn Injuries, 36(5), 647–658. DOI: https://doi.org/10.1016/j.burns.2009.06.199
Miller, K., Rodger, S., Kipping, B., & Kimble, R.M. (2011). A novel technology approach to pain management in children with burns: a prospective randomized controlled trial. Burns: Journal of the International Society for Burn Injuries 37(3), 395–405. DOI: https://doi.org/10.1016/j.burns.2010.12.008
Mirzai, F., Keshtgar, S., Kaviani, M., & Rejaefard, A.H. (2009). The effect of lavender essence smelling during labor on cortisol and serotonin plasma levels and anxiety reduction in nulliparous women. Journal of Kerman University of Medical Sciences, 16(3), 245-254. Available at: https://iranjournals.nlai.ir/bitstream/handle/123456789/249208/55B0747916393C2CFDFD48180E565138.pdf
Morris, L.D., Louw, Q.A., & Crous, L.C. (2010). Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. Burns: Journal of the International Society for Burn Injuries 36(5), 659–664. DOI: https://doi.org/10.1016/j.burns.2009.09.005
Ong, T.L., Ruppert, M.M., Akbar, M., Rashidi, P., Ozrazgat-Baslanti, T., Bihorac, A., & Suvajdzic, M. (2020). Improving the Intensive Care Patient Experience With Virtual Reality-A Feasibility Study. Critical Care Explorations, 2(6):e0122. DOI: https://doi.org/10.1097/CCE.0000000000000122
Osmanlliu, E., Trottier, E.D., Bailey, B., Lagacé, M., Certain, M., Khadra, C., Sanchez, M., Thériault, C., Paquin, D., Côtes‑Turpin, C., & Le May, S. (2020). Distraction in the Emergency department using Virtual reality for INtravenous procedures in Children to Improve comfort (DEVINCI): a pilot pragmatic randomized controlled trial. Canadian Journal of Emergency Medicine, 23, 94-102. DOI: https://doi.org/10.1007/s43678-020-00006-6
Parker, S.I.A., Benzies, K.M., Hayden, K.A. (2017). A systematic review: effectiveness of pediatric peripheral intravenous catheterization strategies. Journal of Advanced Nursing, 73(7), 1570-1582. DOI: https://doi.org/10.1111/jan.13211
Patel, P., Ivanov, D., Bhatt, S., Mastorakos, G., Birckhead, B., Khera, N., & Vittone, J. (2020). Low-Cost Virtual Reality Headsets Reduce Perceived Pain in Healthy Adults: A Multicenter Randomized Crossover Trial. Games for Health Journal, 9(2), 129-136. DOI: http://doi.org/10.1089/g4h.2019.0052
Roshani, B., Rezaei, M., Azadi, P., & Jalilian, A. (2019). The Effect of Binaural Beat Music on Reducing Anxiety and Pain and Increasing Satisfaction of Ophthalmic Ambulatory Surgery Patients. Journal of Kermanshah University of Medical Sciences, 23(4); e99914. DOI: https://doi.org/10.5812/jkums.99914
Scheffler, M., Koranyi, S., Meissner, W., Strauß, B., & Rosendahl, J. (2018). Efficacy of non-pharmacological interventions for procedural pain relief in adults undergoing burn wound care: A systematic review and meta-analysis of randomized controlled trials. Burns: Journal of the International Society for Burn Injuries, 44(7), 1709-1720. DOI: https://doi.org/10.1016/j.burns.2017.11.019
Schlechter, A.K., Whitaker, W., Iyer, S., Gabriele, G., Wilkinson, M. (2021). Virtual reality distraction during pediatric intravenous line placement in the emergency department: A prospective randomized comparison study. American Journal of Emergency Medicine, 44, 296-299. DOI: https://doi.org/10.1016/j.ajem.2020.04.009
Schmitt, Y.S., Hoffman, H.G., Blough, D.K., Patterson, D.R., Jensen, M.P., Soltani, M., Carrougher, G.J., Nakamura, D., & Sharar, S.R. (2011). A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns: Journal of the International Society for Burn Injuries 37(1), 61–68. DOI: https://doi.org/10.1016/j.burns.2010.07.007
Schneider, S.M., Prince-Paul, M., Allen, M.J., Silverman, P., & Talaba, D. (2004). Virtual reality as a distraction intervention for women receiving chemotherapy. Oncology Nursing Forum, 34(1), 39–46. DOI: https://doi.org/10.1188/04.ONF.81-88
Schneider, S.M., Ellis, M., Coombs, W.T., Shonkwiler, E.L., & Folsom, L.C. (2003). Virtual reality intervention for older women with breast cancer. Cyberpsychology & Behavior, 6(3), 301–307. DOI: https://doi.org/10.1089/109493103322011605
Tafazoli, M., Zaremobini, F., Mokhber, N., Emami, A. (2011). The Effect of lavender oil Inhalation on the level of anxiety during first stage of labor in primigravida women. Journal of Fundamentals of Mental Health, 12(4), 720–726. DOI: https://doi.org/10.22038/JFMH.2010.1035
Trost, Z. & Parsons, D.T. (2014). Beyond Distraction: Virtual Reality Graded Exposure Therapy as Treatment for Pain-Related Fear and Disability in Chronic Pain. Journal of Applied Biobehavioral Research, 19(2), 106-126. DOI:https://doi.org/10.1111/jabr.12021
Wolitzky, K., Fivush, R., Zimand, E., Hodges, L., & Rothbaum, B.O. (2005). Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychology & Health, 20(6), 817–824. DOI: https://doi.org/10.1080/14768320500143339
Wong, C.L., Li, C.K., CHan, C.W.H., Choi, K.C., Chen, J., Yeung, M.T., & Chan, O.N. (2021). Virtual Reality Intervention Targeting Pain and Anxiety Among Pediatric Cancer Patients Undergoing Peripheral Intravenous Cannulation. Cancer Nursing, 44(6), 435-442. DOI: https://doi.org/10.1097/NCC.0000000000000844